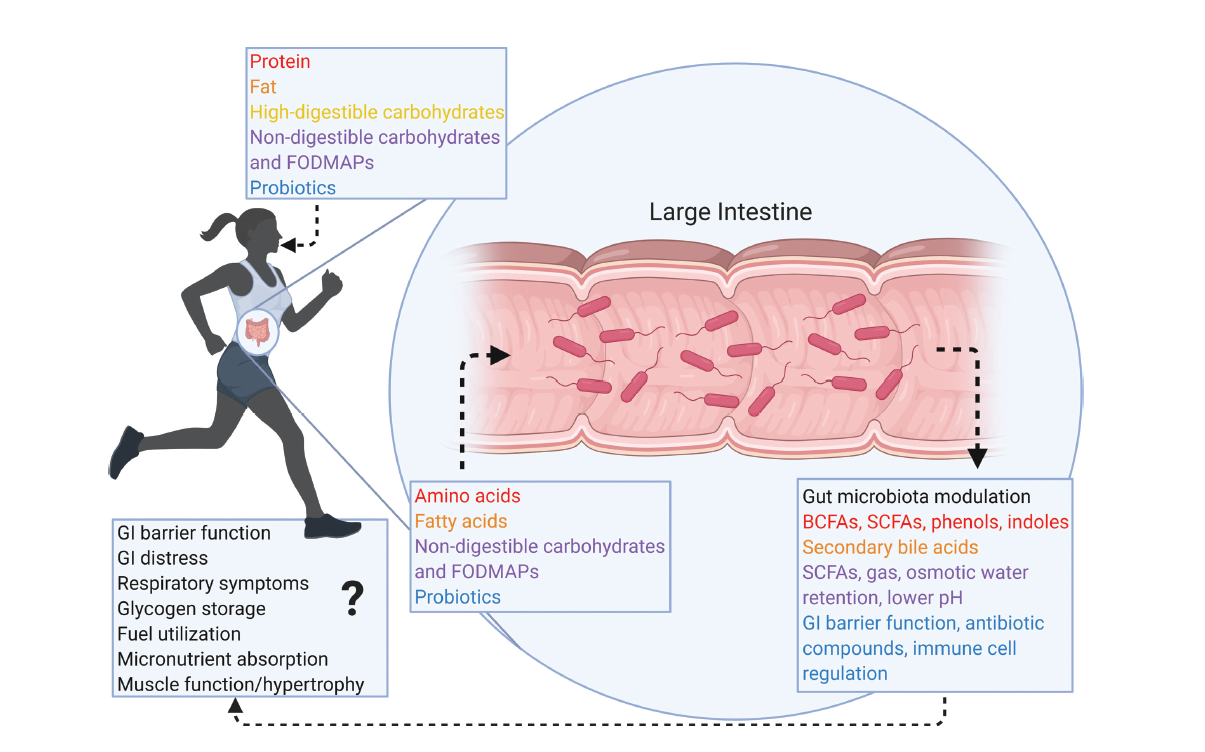
بایدها و نبایدهای غذایی در بیماریهای التهابی روده (IBD) یکی از سوالات اصلی بیماران پس از تشخیص است. اگرچه هیچ غذا یا رژیم غذایی خاصی وجود ندارد که کاملا بتواند از کولیت اولسراتیو و بیماری کرون پیشگیری و یا آنها را درمان کند، تغذیه و رژیم غذایی مناسب می تواند به بهبود علائم و کاهش التهاب روده کمک کند. نشان داده شده است که مصرف سبزیجات، میوه، آجیل، حبوبات، روغن زیتون و منابع پروتئینی بدون چربی مثل لوبیای سویا، گوشت مرغ و ماهی، اثر محافظتی در برابر ابتلا به IBD دارد و به بهبود جمعیت میکروبی روده کمک می کند. در مقابل، الگوهای غذایی غربی، سرشار از اسیدهای چرب غیراشباع امگا ۶، الکل، گوشت قرمز و افزودنیهای غذایی (نمک بیش از حد و شیرینکنندههای مصنوعی) التهاب روده را شدت بخشیده و میتوانند علائم این بیماری را بدتر کنند. به گفته محققین، رژیم غذایی غنی از اسیدهای چرب غیراشباع امگا ۶ (که معمولاً در روغنهای ذرت، سویا، گلرنگ و آفتابگردان یافت میشود) باعث التهاب روده میشود. در مقابل، رژیم غذایی غنی از روغن زیتون و حاوی اسیدهای چرب غیراشباع امگا ۳ (روغن ماهی) و چربی لبنیات باعث تقویت ایمنی در کولیت اولسراتیو می شود.
تغذیه درمانی در شرایط حاد بیماری
در شرایط حاد، بهترین رژیم درمانی ، تغذیه انترال (EEN) است که یک فرمولای مایع است. در این رژیم تمام مواد مغذی ضروری تامین می شود و هیچ غذای دیگری داده نمی شود. این رژیم بخصوص برای کاهش التهاب کودکان موثر است.. در نهایت، EEN باید برای مدت زمان محدودی استفاده شده و سپس غذا به تدریج اضافه می شود.
نتیجه گیری
امروزه رژیم غذایی مدیترانه ای برای افراد مبتلا به IBD که به دنبال یک رژیم غذایی متعادل و سالم هستند توصیه می شود.دانشمندان معتقدند تغذیه و نوع رژیم غذایی افراد IBD باید با توجه به شدت بیماری و آنچه در سبک زندگی آنها اتفاق می افتد، شخصی سازی شود. بنابراین مشاوره با یک متخصص تغذیه با تخصص در مدیریت IBD برای ایجاد یک برنامه فردی ضروری است. توصیه می کنیم قبل از انتخاب یکی از رژیمهای غذایی مد روز که بعضا بصورت آنلاین تبلیغ میشوند، با پزشک خود صحبت کنید تا شما را به یک متخصص تغذیه وارد در این بیماری معرفی کند و یک برنامه غذایی شخصیسازی شده برای شما تجویز شود.
مترجم: راحم رحمتی(Rahem Rahmati)- نازیلا کسائیان(Nazila Kassaian)
ویراستار: مرضیه رحیم خراسانی (Marzieh Rahim Khorasan) – پریسا هاشمی ( Parisa Hashemi)
References
- Palumbo VD, Romeo M et al. (۲۰۱۶), The long-term effects of probiotics in the therapy of ulcerative colitis: A clinical study. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub; 160(3):372-377.
- Rodolico V, Tomasello G et al. (۲۰۱۰), Hsp60 and Hsp10 increase in colon mucosa of Crohn’s disease and ulcerative colitis. Cell Stress and Chaperones vol. 15, 877–۸۸۴.
- Bellavia M, Tomasello G, Romeo M et al. (۲۰۱۳), Gut microbiota imbalance and chaperoning system malfunction are central to ulcerative colitis pathogenesis and can be counteracted with specifically designed probiotics: a working hypothesis. Medical Microbiology and Immunology vol. 202, 393–۴۰۶
- Tomasello G, Sciumé C et al. (۲۰۱۱), Hsp10, Hsp70, and Hsp90 immunohistochemical levels change in ulcerative colitis after therapy. Eur J Histochem; 55(4):e38.
- Tomasello G, Palumbo VD et al. (۲۰۱۴), Probiotics and conventional terapy: new fronter in therapeutic approach in articular manifestations of IBD. Progress in Nutrition 2014; Vol. 16 N. 3: 176-187